My collision with the neurological autoimmune condition of CRPS began while sitting in my knee surgeon’s office three years ago. Complex Regional Pain Syndrome, formerly known as Reflex Sympathetic Dystrophy (RSD), is an often misunderstood and hard to diagnose condition in which pain lingers after the initial injury has healed.
According to Dr. Robert Schwartzman, a leading doctor in the field of CRPS treatment, millions of people in the United States suffer from the condition and it can affect anyone, even children.
There I sat with my husband in tow, waiting for some kind of verdict for this mysterious, aggravating, and abnormal pain. I’d been having this pain since I injured my knee in a non-combat incident while deployed with the U.S. Air Force overseas a year earlier. So, as this newest knee specialist, apparently one of the top knee surgeons in the country, gazed over my recent MRI, I wasn’t very hopeful that he would be able to give us a definitive answer. The other six orthopedic doctors both in the U.S. and overseas I had been to didn’t have any answers. I thought, so, why should this guy?
The first thing Dr. Frank Noyes of the Cincinnati Orthopedic Center said was completely expected. He said my kneecap was shredded and would need to be replaced.
OK, I already knew that, I thought. I’d been getting the runaround and had been doing a lot of research on my own. Since the initial injury in 2012, Air Force medical staffers and the orthopedic specialists at the Dayton, Ohio Veterans Affair (VA) in their infinite wisdom had told me over and over that nothing was wrong. It’s just a sprain, they said. Put some ice on it, they said. Take some Motrin, they said. Here’s a Hyalgan shot or two, that’ll fix it, they said. Nothing they suggested worked.
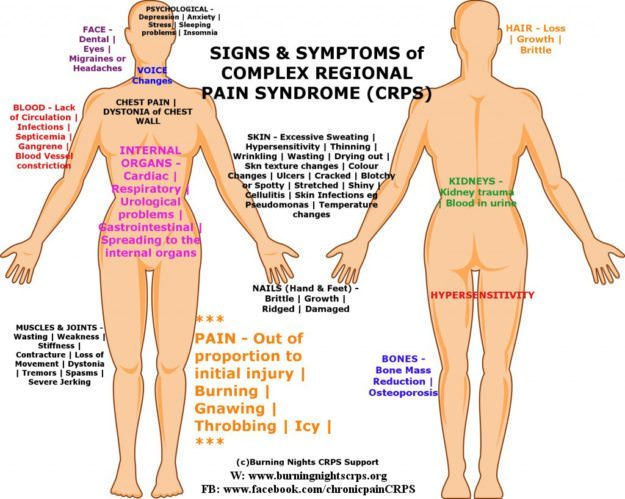
In the affected part(s), CRPS manifests itself as aching, cold and burning with skin sensitivity, as well as a sharp shooting pain at times. My knee would often turn bright red and swell up to three-times the size for days without any reason. Standing, walking, and sitting for long periods would aggravate it. As time went by without a diagnosis or proper treatment, the pain and dysfunction became so bad that I could barely walk. My right knee was now presenting with a valgus deformity, meaning that my kneecap was turned inward, causing my gait to be crooked.
The valgus deformity completely threw my Air Force doc off. He didn’t know what to do with me so he sent me to his mentor, Dr. Noyes.
After muttering something intelligible to the nurse, Dr. Noyes said something that totally threw me. “We cannot do any kind of scope to confirm the damage or surgery to fix it until we get your CRPS in check.”
Restore Balance And Health With The World’s Most Prominent Supplement Kit
CRPS What?
My, what? I thought. What is he talking about? Is this yet another misdiagnosis? I wondered. But no, I’m not at the VA. This guy is supposed to know what he is talking about.
“What’s that?” My husband piped up before I could say anything. Dr. Noyes explained to us what it was. It’s an autoimmune condition often caused by an injury or as a result of surgery.
There are several antidepressants and anticonvulsants which can control it such as gabapentin, topical local anesthetic creams, and patches such as lidocaine, Lyrica and Cymbalta, he said. But a pain management specialist would be needed to figure out what would work to properly manage it, he added.
He then explained that any kind of surgery could cause it to spread and make it worse. This is why he refused to schedule surgery until it was under control.
I was referred to a pain management specialist and participated in many rounds of physical therapy before Dr. Noyes scheduled any surgery to fix the initial problem. In the past two years, I have had two knee surgeries, one being a kneecap replacement. The CRPS has been kept at bay with the Cymbalta and physical therapy until recently.
CRPS can also appear as a itchy rash, unexplained bruises, or other inflammation and can manifest itself all over the body. In fact, the other day I woke up with a black eye. I had not been touched by anyone or anything. In 24 to 48 hours, it will be gone. I’ve had this happen to my toes, fingers, both knees, arms, and legs.
According to the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institutes of Health (NIH), CRPS is believed to be caused by damage to, or malfunction of, the peripheral and central nervous systems. CRPS represents an abnormal response that magnifies the effects of the injury with the most common triggers being fractures, sprains/strains, soft tissue injury (such as burns, cuts, or bruises), limb immobilization (such as being in a cast), or surgical or medical procedures (such as needlestick).
The NINDS states that people with CRPS have peripheral nerve abnormalities usually involving the small un-myelinated and thinly myelinated nerve fibers that carry pain messages and signals to blood vessels. Because small fibers in the nerves communicate with blood vessels, small nerve fiber injuries may trigger the many different symptoms of CRPS. Molecules secreted from the ends of hyperactive injured small nerve fibers are thought to contribute to inflammation and blood vessel abnormalities. These peripheral nerve abnormalities in turn trigger abnormal neurological function in the spinal cord and brain, leading in some cases to complex disorders of higher cortical function.
According to the NINDS, another abnormality in CRPS involves the blood vessels in the affected limb, which may dilate (open wider) or leak fluid into the surrounding tissue, causing red, swollen skin. The underlying muscles and deeper tissues can become starved of oxygen and nutrients, causing muscle and joint pain and damage.
Drugs, Physical Therapy, And Other Modalities
Not much is known about this condition and treatment involves a lot of trial and error. After trying gabapentin and Lyrica along with ongoing physical therapy throughout my conventional knee treatments, we found that the anticonvulsant drug Cymbalta is yielding positive results.
The pain and unexplainable inflammation doesn’t ever go away completely, but I am considered in medical circles as “well-managed” in regard to this condition.
I am still subject to flare-ups, especially after exercise. I use an e-stim (TENS) machine to alleviate the acute pain and swelling. Heating pads and ice usually do not work for a CRPS flare-up. My physical therapist has advised me not to use the e-stim over ice because ice can make the flare-up worse and can even lead to the spread of the disease.
An e-stim or TENS machine can be ordered through your orthopedic surgeon, pain management specialist, or physical therapist. According to WebMD, transcutaneous electrical nerve stimulation (TENS) is a therapy that uses low-voltage electrical current for pain relief.
As with most CRPS treatments, most insurance plans cover very little of the cost of the machine and some plans do not cover it at all. I am a Post 9/11 veteran so I have to go through the VA. The VA’s procedures to get a TENS machine are so convoluted that I ended paying out of pocket for my machine, which was ordered through my physical therapist. But for flare-ups, it is so worth it.
CRPS can spread if not held in check. Those who suffer from this condition are at risk of it spreading if they have any subsequent injuries or the drug therapy reaches a plateau and stops working. Most commonly it will spread from the affected limb to another.
According to researchers at the International Research Foundation for RSD/CRPS, studies have shown that Ketamine infusions have been reported to be safe and effective for the management of CRPS in both the inpatient and outpatient settings. Ketamine is a tranquilizer and is administered in a hospital setting over a period of five days via intravenous infusion. The treatment does not work for everyone and more often than not, insurance plans will not cover it.
Trying Just About Anything
For those in which drug therapy alone does not manage their conditions fully, alternative treatments can be explored. Believe me, when you are in pain 24/7, you will try anything to make it go away even if it is short-lived relief. Cannabis is a newer alternative treatment which I have not yet personally tried as I live in a state where the drug is still illegal. But I have tried Reiki, meditation, acupuncture, yoga nidra, Bikram yoga, warm water therapy, acupressure (pressure on certain nerves to gain pain relief) and fascial release.
What works for me won’t work for the next person with CRPS. No one case of CRPS is the same. It affects each person differently. You just have to keep trying different things to see what works best for you. Hot yoga didn’t work for me but meditation coupled with Vinyasa yoga does. Yoga nidra and meditation helps me sleep at night and the TENS therapy along with acupressure helps with my flare-ups. All this is in addition to the daily Cymbalta and physical therapy regimen.
A new promising therapy that has helped some CRPS sufferers is Manual Ligament Therapy (MLT). MLT was developed by Arik Warren Gohl, a medical manual therapist from Tacoma, Wash. MLT is much like acupressure but it is applied to targeted ligaments. He calls this therapy the Gohl Program.
Where To Turn For Support
What has been more helpful than anything in my journey through the pain of CRPS is the wealth of online support that is out there. The Facebook groups I rely on for tips and advice on a daily basis are:
All are closed groups so you will have to request to join each community.
The following pages provide more general information on new treatments, coping strategies, and advice.
- RSD/CRPS Chronic Pain
- CRPS Help Tips
- RSD/CRPS Doesn’t Own Me
- RSD/CRPS Supporting each other
- RSD/CRPS Friends In Pain
- Surviving CRPS & Chronic Pain, Our Personal Journeys
Another website with a wealth of information is the Definitive Library for RSD/CRPS/ChronicPain It’s not a pretty interface but if you can get past that, it includes links to all the most updated research on new treatments, advocacy information, and financial advice for those who are under insured and can’t afford treatments.
 Stefanie Hauck is a Post 9/11 Air Force combat veteran and freelance journalist. She lives in Delaware, Ohio, with her husband, Matt, and two children. She was diagnosed with CRPS in 2013 from injuries sustained while deployed in 2012.
Stefanie Hauck is a Post 9/11 Air Force combat veteran and freelance journalist. She lives in Delaware, Ohio, with her husband, Matt, and two children. She was diagnosed with CRPS in 2013 from injuries sustained while deployed in 2012.
Submit your story or essay to Buzzworthy Blogs.
Editor’s Note: HoneyColony does not support the use of antidepressants as a long term solution to an autoimmune condition. We believe in alternative natural forms of treatment.





1 thought on “My Journey Living With A Rare Autoimmune Called CRPS”
thank you soo much for sharing your story. ears to toes of this horrible pain for three years now. I at least feel validated. and bless you for serving.
Comments are closed.